A few days before Thanksgiving, my oldest brother Peter suddenly and unexpectedly passed away. Peter was amazing, setting an example for me and so many others. We all dearly miss him. This is a cruel reminder of how important it is to spend time with those close to us and make sure they know how much we love them. Please take the opportunity during this holiday season to embrace family and friends.
Complementing his distinguished record of public service, my brother Peter was dedicated to initiatives that improved patient safety in his work as an executive at a medical malpractice trust. Although Peter was trained as an attorney rather than a physician or clinical epidemiologist, he understood complex studies related to the delivery of health care, asked excellent questions suitable for scientific investigation, and provoked thoughtful deliberations in our many discussions. Peter always wanted to learn and loved information from all kinds of studies: those of small groups of patients that enable detailed examinations of specific treatments as well as those of national treatment patterns that inform broader discussions of health care quality and access.
Patients with sleep apnea are not seeing otolaryngologists to consider surgery
The December 2012 issue of Otolaryngology—Head and Neck Surgery included an article (and a podcast now uploaded) in the latter category that examined the epidemiology of office visits related to obstructive sleep apnea in the United States. In 2008-2009, there were an estimated 4.1 million office visits annually in the United States related to obstructive sleep apnea. Of these, about 10% were to otolaryngologist—head and neck surgeons (aka ear, nose, and throat doctors). This study is important because this 10% figure is lower than one would expect, given that surgeons are able to diagnose, initiate treatment (whether or not Board-certified in sleep medicine), and discuss potential surgical options.
What otolaryngologists do for snoring and sleep apnea
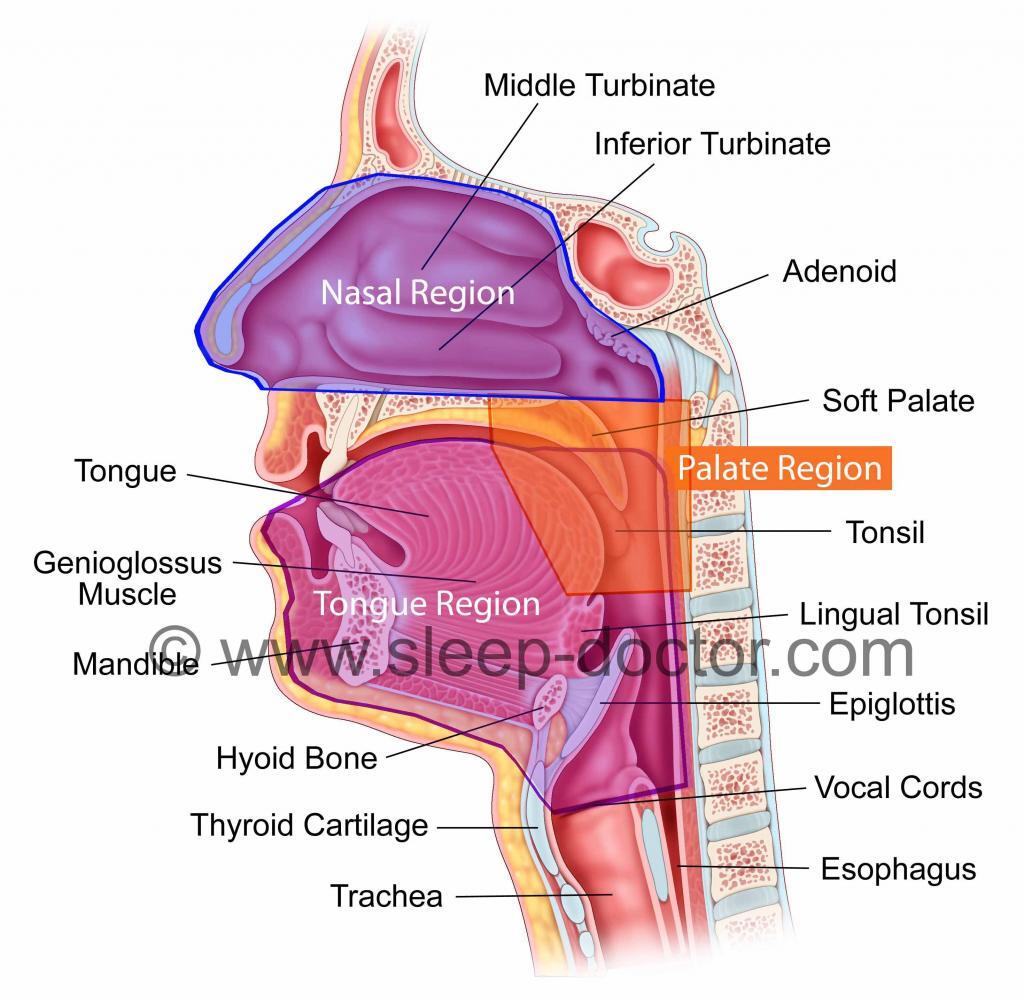
A patient with snoring or obstructive sleep apnea might see an otolaryngologist—head and neck surgeon for a few reasons. Often I provide the initial evaluation and can identify factors that should be addressed before considering a test for sleep apnea, called a sleep study. Performing a detailed history and physical examination of the nose and throat is essential to identify easily-treated conditions that can cause snoring or sleep apnea. Otolaryngologists specialize in head and neck surgery and are best positioned to examine the areas of the body that are responsible for snoring and sleep apnea in most patients.
If a patient has snoring without sleep apnea, an otolaryngologist-head and neck surgeon is best positioned to offer surgical and non-surgical treatments of the head and neck. Often, it can be as simple as treatments to do at home, as described in a previous blog post. However, palate stiffening procedures like the Pillar Procedure, can provide a substantial reduction or eliminate snoring in certain types of patients, based on selection after an examination in the office.
Finally, I see patients with sleep apnea who are referred after either being unable to tolerate positive airway pressure therapy or after previous surgery that does not alleviate their sleep apnea. It is commonly argued that surgery for sleep apnea does not work. That is simply not true. Although the most common surgery for sleep apnea, a soft palate procedure called uvulopalatopharyngoplasty, does not resolve sleep apnea in many patients, it has been shown to provide substantial benefit, often similar to positive airway pressure therapy, in the highest-quality study that followed large groups of Spanish patients with sleep apnea over time.
Surgery for sleep apnea is not limited to this one procedure alone. My research has focused on identifying the factors contributing to snoring and sleep apnea, and it is well-established that using the same treatments for all patients is doomed to failure. There are a number of providers—sleep medicine physicians, otolaryngologist—head and neck surgeons, and dentists—that advertise heavily aand offer a single option to patients, but everything we know about snoring and sleep apnea indicates that this is doomed to failure because people are different. Surgical procedures enlarge and stabilize different structures around the airway to treat snoring and obstructive sleep apnea. There are three major areas that can contribute to these conditions: the nose, palate, and tongue regions. In an individual patient, often more than one of these areas are responsible. Addressing these areas in a targeted yet appropriate fashion improves outcomes. Careful patient evaluation represents a critical opportunity to develop a personalized treatment plan and achieve the best results.
Why does it matter if patients see otolaryngologists?
Many patients who do not tolerate positive airway pressure therapy currently go untreated. This is not acceptable. Whether patients with sleep apnea are sleepy or fatigued or whether they have potential serious health risks (especially true for those with moderate to severe sleep apnea), many patients are told that positive airway pressure is their only option and never see another provider if they cannot tolerate it. The important thing to know is that there is more that can be done. The first step is to learn why someone cannot tolerate positive airway pressure therapy. Simply not liking a machine is not a good-enough reason to consider surgery, but often there are some simple things that can be done to improve usage of positive airway pressure therapy. Some of my happiest patients are those who have blockage of breathing in their nose and find it uncomfortable to wear a mask that blows air through the nose until they have their nasal passages opened.
What should I do if have snoring or sleep apnea?
Sleep disorders can be treated by a variety of providers: sleep medicine physicians, sleep surgeons (typically otolaryngologist—head and neck surgeons but also oral and maxillofacial surgeons), and sleep dentists. Patients benefit from having providers who are aware of the range of treatment options, starting with conservative treatments and going from there. So seek out providers that work with colleagues from other specialties who are dedicated to making sure every patient gets treated properly, independent of their own area of expertise. We want to avoid the cliché of “When you have a hammer, you look for nails” that leads individual providers, working in isolation, to promote the only treatment they offer. Because patients today are so educated (and I hope this blog and website help), it is important to make decisions with patients rather than for patients. Patients often report that providers have made absolute statements like “positive airway pressure is the only treatment for sleep apnea”, “surgery does not work”, or “XXX procedure is the only one that works”. All of these statements are wrong. Snoring and sleep apnea are just like any other medical condition. Treatment requires an option that works and that patients will accept.



57 − = 47