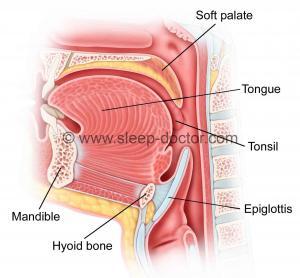
As you can probably tell, I truly enjoy sharing ideas with colleagues and patients about some of the challenges we face in treating snoring and obstructive sleep apnea. One topic that provokes particularly intense discussion is the role of the epiglottis in sleep apnea. My colleague, Dr. Andrew Goldberg, came up with the title for a lecture I have given (and which I have used for this blog post), based on the notion that the epiglottis protects us from hazards but also can be a primary cause of obstructive sleep apnea. The epiglottis (see illustration) is a piece of cartilage, covered with mucosa (lining of the throat), that sits in the lower part of the throat, where its major role is to assist in swallowing. During swallowing, the muscles of the throat push the epiglottis backwards (in addition to other throat movements) to cover the voice box (larynx) during swallowing and prevent food and liquid from entering the lungs.
Based on our research utilizing drug-induced sleep endoscopy and the work of others, it is estimated that about 10% of patients with sleep apnea appear to have their epiglottis substantially either fall backwards or fold in half during sleep. Both of these can narrow the space for breathing and contribute to sleep apnea. For patients with sleep apnea and the physicians who treat them, there are two questions:
- What is the best way to determine if the epiglottis is playing a role?
- How do we treat the epiglottis?
Identifying the epiglottis as an important factor in sleep apnea
There are many evaluation techniques for patients with snoring and obstructive sleep apnea. I have completed a number of studies related to drug-induced sleep endoscopy because I think it offers unique insight into what is causing blockage of breathing during sleep. When done carefully, this evaluation may reproduce a sleep-like state that allows us to examine what structures in the throat may be contributing to sleep apnea. This is very different from most other techniques, which are performed with patients awake. Identifying the role of the epiglottis may be a very important role for sleep endoscopy, as other evaluation techniques are unable to determine this.
Because drug-induced sleep endoscopy has some risks and costs, many of us who have tried to determine other ways to obtain the information we get from sleep endoscopy without the risks and costs. I have noticed two things in patients where the epiglottis plays an important role. One is that these patients may get a sensation of choking with their continuous positive airway pressure (CPAP) therapy, which is not only dramatic and disturbing but which is very different from other reasons for being unable to tolerate CPAP. This may occur because CPAP could, at least theoretically, be pushing the epiglottis backwards to create a complete seal in the throat that cannot be relieved by higher CPAP pressures. This is very different from blockage due to other structures like the soft palate or tongue, where blockage is relieved when the CPAP pressure rises. The other findings common to many patients with an epiglottis role come from the fiberoptic telescope that I use to examine patients in the office. The epiglottis can often be sitting further back, almost positioned against the back of the throat, and often there is a curve to the upper half of the epiglottis, almost as if it is bent forward (towards the tongue) over time, as the epiglottis is repeatedly falling back against the back of the throat. Relying on these findings have not replaced drug-induced sleep endoscopy in my practice, but they can make me suspicious about a role for the epiglottis.
How to treat the epiglottis in sleep apnea surgery
Once we suspect a role for the epiglottis, whether from drug-induced sleep endoscopy or some other evaluation, what should we do? As described above, increasing CPAP pressures may only make the problem worse. Decreasing CPAP pressures also will not work, as there often needs to be enough pressure to open the breathing passages. So we must look at alternatives, either to address the sleep apnea by themself or in combination with treatments like CPAP. Behavioral changes like weight loss, avoiding sleep on one’s back, and eliminating alcohol intake within 3 hours of bedtime will likely help many patients, but they are not specifically targeted to the epiglottis. Oral appliances move the lower jaw forward and can also be very beneficial, but they also do not address the epiglottis directly. Although surgery is not the only option for these patients, it is the only category of treatment that can focus on the epiglottis.
The two major types of procedures that are directed more specifically at the epiglottis are removal of a portion of it (partial epiglottectomy) and hyoid suspension. European colleagues have substantial experience with epiglottis surgery, but the two major published studies (brief summaries here and here) of the procedure come from a collaboration between surgeons in New Jersey and Israel. They selected patients with one of the findings mentioned above (positioning of the epiglottis towards the back of the throat during awake physical examination in the office) and performed a somewhat-aggressive removal of part of the epiglottis. Their approach produced dramatic improvements, clearing up sleep apnea in almost 80% (21/27) of those in one study. In Europe, this is a common approach for patients who have an epiglottis contributing to sleep apnea; although my colleagues tell me their results are very good, there are no other studies reporting on results with this procedure alone. Personally, I have been concerned about being so aggressive because of the risks of having food or liquid fall into the lungs when attempting to swallowing, but my results have not been as impressive as theirs.
The hyoid suspension procedure treats the epiglottis differently. The hyoid bone is a relatively thin, horseshoe-shaped bone in the neck. The hyoid bone in humans is unique in that it can move. A mobile hyoid bone appears to have been one of the evolutionary changes important in the development of speech, but it likely also contributes to our risks for developing sleep apnea (which is not seen in most animals, except for some dogs). The hyoid bone is important in sleep apnea because it has attachments to a number of other structures, including the epiglottis (through the hyoepiglottic ligament) and muscles that are next to or surround the throat (including the middle pharyngeal constrictor). During sleep, muscles relax, and the hyoid bone is free to move towards the back of the throat, allowing the structures attached to it to fall into the throat and block breathing. The hyoid suspension procedure involves pulling the hyoid bone forward and using stitches to secure the hyoid bone either to the top part of the Adam’s apple (thyroid cartilage) in a slightly-downward direction or to the lower part of the lower jaw (mandible). These hyoid suspension techniques have not been compared side by side, but we completed a study in a small number of human cadavers that compared pulling the hyoid bone forward in different directions. This study suggested that the best direction may be directly forward, closer to the suspension to the thyroid cartilage. This is the hyoid suspension technique that I use in my own practice.
What do I do if I am worried about the epiglottis?
I believe strongly that the epiglottis plays an important role for about 10% of patients with obstructive sleep apnea. There are clues from the medical history and physical examination that make me more or less concerned about this, but the main way I check for the role of the epiglottis is with drug-induced sleep endoscopy. I have had success treating these patients using both partial epiglottis removal and hyoid suspension. In speaking with my patients, we combine specific findings from their examination as well as their preferences (these procedures have slightly different risks and characteristics) to develop a joint decision about the best option for them.




Steven Wu says:
Hi, Eric:
Thank you for your sharing about the epiglottic obstruction-related apnea. It’s reaIIy pearl and important to sleep surgery! I think now my favorite is reading your article and learn more real-time knowledge that can improve me to clinical treat OSA. My question is how about laser trimming to lingual side of epiglottis, like laryngomalacia treatment? Is it work? Thank you!
Dr. Kezirian says:
It can work, but it is not something to apply uniformly to patients with epiglottic obstruction, in my opinion. The European surgeons I know use it more than I do, as I will often perform hyoid suspension or consider other options to treat the epiglottis.
Tim Ryan says:
I was treated for cancer 12 years ago with radiation and cemo to my neck. It has shrunk my opeglottis and now I am asperating food into my lungs. Is there a treatment to help my opiglottis to function like it should.
Dr. Kezirian says:
You should talk with the team that has been treating you. Often speech therapy can make a dramatic improvement in swallowing. There are other potential treatments too.
Chris Duran says:
Hello,
After five ENTs, and just as many throat and sinus surgeries, I think i have finally gotten the source of my sleep breathing problem narrowed down to my airway around my epiglottis.
I am finding that I am being told that “CPAP should work if this is your problem”–I have CPAP, but despite persistant tries, I cannot get it to help (it feels like I’m choking even more).
I have demonstrated to two doctors that my airway shuts easily when I’m not keeping my throat muscles flexed, but it’s hard to demonstrate that I am not deliberately doing it and that I am simply relaxing my muscles.
My questoin is–are you aware of any ENTs or sleep doctors who specialize in this exact part of the throat with respect to sleep problems? My four sleep tests have all shown no deep sleep, very mild sleep apnea, but severe counts of respiratory arousals.
The one complication is that I did have a hyoid suspension–which helped a little bit, but I suspect it may be the muscles around my epiglottis and not the actual thing causing the problem.
Any referral or recommendation would be appreciated!
Thank you,
Chris
Dr. Kezirian says:
I am not sure exactly how you have identified the epiglottis as the cause of your sleep apnea. There are a few options and some people to see. I am ot sure where you live, but I do see people that travel to see me. If this interests you, please feel free to e-mail me directly.
Brandon says:
Dr. Kezirian,
What are your thoughts on the partial epiglottectomy vs. epiglottopexy?
Would love to hear if you prefer one or the other and why.
Btw, you have an outstanding blog.
Dr. Kezirian says:
Thank you for the kind words. I do not performed isolated epiglottopexy, although I do feel that I get something like that when I perform tongue base resection. For isolated epiglottis treatment, I would be more likely to perform partial epiglottectomy.
Ryan says:
Dr. Kezirian,
I seem to fall in the same category as Chris. Almost exactly, except without the hyoid suspension. My epiglottis closes and partially obstructs air when I’m sleeping. I can voluntarily close it at any time (shown to several doctors), and have tried unsuccessfully for years to fix it (sinus surgery, acid reflux studies, etc.). As an ENT is suggesting another sinus surgery, do you feel there is a link between sinus blockage, and floppy epiglottis? It seems to be related to the pathways of air when I’m breathing. I can tell myself to breath one way, and can’t close it. Another way, and I can. When I’m relaxed, I’m more prone to breath the way that closes it. I’m trying to decide if another sinus surgery would help this problem.
If you have experience with this sort of thing, I would be willing to travel to see you, as I’m desperate for answers.
Thank you.
Dr. Kezirian says:
This would be unlikely to be related to sinus issues. There are some epiglottis-directed procedures, whether removing a portion of the epiglottis or performing a procedure called hyoid suspension. You can contact me directly via e-mail at [email protected] with additional questions, and I would be happy to see you as a patient.
Tim says:
I just came back from my findings from a drug-induced sleep endoscopy and it is clear that my epiglottis is closing over and over again as I sleep. As we look to schedule surgery for partial epiglottis removal, I am looking over the internet for recovery times, anecdotal stories, and also the short and long term expectations for swallowing adjustments. My wife wants me to find out especially about swallowing as I get older, as older people tend to asphyxiate more easily. I am only 40 now, so not an issue right away, but obviously will be at some point. Can you tell me more about recovery or point me in the right direction?
Dr. Kezirian says:
You raise some good questions, and the answers are clearly getting into the realm of medical advice. Honestly, these are questions you should ask your surgeon. The issue with getting older is not asphyxiation (lack of air) but more either aspiration (food/liquids going the “wrong way” into your lungs) or jsut other trouble with swallowing.
Robert says:
Hi Eric,
Are you aware of anyone who tried to fix epiglottis obstructions with electric stimulator like Inspire? Is it possible in theory?
AFAIK, there are studies that identified that complete concentric collapse of the palate is a common cause of failure to achieve cure, but not a word about epiglottic obstruction.
Dr. Kezirian says:
Upper Airway Stimulation can work with epiglottic obstruction, but it is not obviously clear one way or the other. Epiglottis-related obstruction is not one of the reasons to exclude someone from getting Upper Airway Stimulation. I have definitely had patients who have had good responses and have not seen epiglottis-related obstruction as a reason for failure.
Jason lui says:
Dear Dr. Kezirian,
I was diagnosed with OSAS since my late 20s. I was unable to adapt to the CPAP therapy for some unknown reason. My surgeon said my epiglottis has curled Inward during sleep and therefore performed a UPPP and hyoid suspension to me . Unfortunately, The result was not satisfactory as I expected. I still cannot has good sleep even with CPAP. I don’t feel that the air from CPAP has expanded my airway. My every breathe still need effort even I have put on the mask.
Later, I saw another surgeon and he said CPAP compliance issue maybe due to my congested nose. He later performed a inferior turbinoplasty to me. The problem Improved a little only in the beginning. I still could not adapt to CPAP up to now.
For years I have tried numerous ways to help me sleep better such as using dental appliances , or the Provert therapy. The effect were all inconsistent. I’m 35 now, I have been having no idea what’s wrong with me until I saw your blog. The problem is still related to the epiglottis. May I know ,base on statistic, is the hyoid Suspension an effective surgery to address the epiglottis problem. Did you see any case in which hyoid suspension did not help improve the problem?
Thanks for your kindly reply.
Dr. Kezirian says:
It is not 100% clear what surgical approach is best for epiglottis-related obstruction. In some cases, hyoid suspension has worked well for me, but I have also performed epiglottis surgery (partial removal) with success. Neither one is perfect for all patients, so one could perform drug-induced sleep endoscopy to evaluate you at this time. Eric
Jason Lui says:
Is it more likely that epiglottis-related obstruction can caused UARS instead of OSAS ? My recent PSG sleep study show RDI 5 but with 24 spontaneous arousal per hour. CPAP usage also report a <5 AHI.
Dr. Kezirian says:
Anything that causes obstructive sleep apnea can cause what many people call upper airway resistance syndrome but which has been generally reclassified as a type of obstructive sleep apnea. This includes the epiglottis.
Jason Lui says:
Dear Dr. Kizirian,
In the case of epiglottis blocking airway in CPAP therapy, could the CPAP machine report any abnormal usage statistic (e.g. high AHI,high flow limitation) that could help you identify the problem in epiglottis ??
Dr. Kezirian says:
There is nothing specifically that would show this, to my knowledge. This is why it is difficult to identify. In my experience, this sensation of choking due to CPAP is the most common thing I see when someone has the epiglottis playing a role.
Christina LeMieux says:
Hi. I was recently diagnosed with OSA. the results were surprising to me as I have a borderline to normal BMI and my sleeping partners in my life always reported that while I snored, there was never any apnea that they could tell. However, the diagnosis made perfect sense in light of my daytime symptoms. I do recall most of my life waking up stuck on an exhale and having to do a maneuver in the back of my throat to let the air out. Never on an inhale that I or my boyfriend can recall. Now that I am using CPAP for the last week, it is dramatically worse, though the ‘sleep coach’ I spoke to said during the hours I’m wearing the CPAP my instances of apnea are decreased. Also, I have no chronic respiratory issues, but using the CPAP has left me congested and wheezy for hours after use. I am on a setting of five. I have an appointment in one week with the DME co. to change to a FFM, and a follow up appointment with my sleep doctor in a few months. I cannot see where the FFM would be helpful as my problem seems to be overcoming the positive air pressure on exhale, and even when I’m not having to fight the positive pressure. Are my symptoms typical for what you see in somebody with an epiglottis issue? I asked because my doctor and my area ( the North SF Bay area) do not offer the drug induced endoscopic diagnostic test. Also, my doctor seems to be pretty resistant to the idea of surgery, even failing CPAP. I may have to travel to get something done.. But I would feel much better undertaking something like that if I knew that my chances were good that I have something that would respond favorably to surgery. I do also have a very long uvula and a torus palatinus, if that helps. But again, never any issue choking on an inhale, but often on an exhale. My sleep study was done at home , if that makes any difference? I would appreciate any input you are able to give. Thank you, Christy
Dr. Kezirian says:
It is always a good idea to have a thorough trial of conservative approaches like CPAP. However, if CPAP is not working well for you (including if you are not sleeping comfortably with it), then you should consider surgery and/or oral appliances. I would recommend seeing a sleep surgeon. There are some in the Bay Area, and I would also be happy to see you. If you would like to discuss this in more detail, please feel free to send me an e-mail to [email protected].
Emily says:
Hello!
I found this article very interesting. I have complex sleep apnea with severe central sleep apnea. I don’t really choke in my sleep as much as my brain just doesn’t tell me to breathe. I do have mild obstructive sleep apnea as well though. My epiglottis is actually visible by looking into my mouth. Could the high rising epiglottis play a part in the obstructive sleep apnea? I’ve never had any known issues with it but have always wondered if it is related.
Dr. Kezirian says:
A high-riding epiglottis is not a problem by itself, and it would not cause central sleep apnea.
Ravi says:
I had a prolapse epiglottis diagnosis observed while doing a deviated septum correction (which I got while taking a stab in the dark at trying to do anything that could possibly improve my sleep). CPAP definitely improves things considerably, but the choking sensation can still be there and CPAP also kills my wife’s sleep. Unfortunately, my home sleep test AHI was too low (7.8) to qualify me for hyoid suspension insurance coverage. I’m trying to get a lab test approved on the possibility that would return a higher AHI, but overall just trying to learn what my options are. Are you able to do remote consults for initial discussions (in S.F. so could come down to L.A. for any procedures, but it’s a bit far for the consults too)
P.S. many thanks for your articles!
Dr. Kezirian says:
I am available for Skype consultations. Please e-mail me directly at [email protected].
Rosemary Laidlaw says:
I’m a 76 year old female who was diagnosed with OSA over 25 years ago. I always use my CPAP machine and have spent years trying to work out what is actually blocking what.
This may not be science in the form experts know it but I think useful anyway.
Sometimes when sleeping part of my brain wakes up and a form of ‘Sleep Paralysis occurs. Over time I’ve trained myself not to panic and fight to awake properly and observe what is going on.
In my case and I’m 100% positive now is that my Epiglottis is responsible for my Apnoea. It also explains during REM sleep when I’ve checked my machine why the air pressure rises from 7 to 9. At certain times.
I have quite a low tone of voice and many times over the phone been called Mr !!!!
Just thought this information would be useful in the ongoing studies of OSA.
Will says:
Hello,
I was recently diagnosed through DISE as having isolated epiglottis collapse. It was also found by CT that my epiglottis falls back against my posterior airway. I have been trying EPAP for one week now with no obvious enhancements to sleep. I’m wondering if I would be a good candidate for some form of surgery?
Dr. Kezirian says:
If it really is EPAP (Provent) that you are trying, then unfortunately that is not super likely to work for this. CPAP can, but actually sometimes it can make things worse. It is not 100% clear what surgery would be best for you, as some patients could benefit from partial removal of the epiglottis, while a procedure like hyoid suspension might be better for others.
Will says:
Sorry, I meant CPAP, my mistake. Thanks for the feedback~
Will says:
Hello,
I posted above with a question regarding treatment for epiglottic collapse. I was told by surgeons where I live that the risk of aspiration post-surgery is too high and that the surgery should be avoided at all costs? I was wondering what Dr. Kezirian’s experience is on this subject? Is there really a high risk of aspiration in patients who have had partial-epiglottidectomy? Thanks.
Dr. Kezirian says:
Thank you for e-mailing me directly on this. I will copy the answer I provided to you:
Nobody knows for sure. The risk of aspiration likely increases with the amount of epiglottis resection and the age of the patients. Overall, there is probably low-grade (not apparent to patients and not meaningful) aspiration in more patients than we think, but the risk of anything notable is probably below 5%.
Gaurav Dhakal says:
Is overhanging epiglottis same as a floppy one ? I have OSA and use CPAP. It does not help much but a I also had a feeling of “something” in my throat. could it be the overhanging epiglottis that I feel , and most probably my glottis is also causing my apnea.
Dr. Kezirian says:
I am not sure entirely what is meant by an overhanging epiglottis, but this can be occurring if your epiglottis is positioned towards the back of your throat in general. A feeling of something stuck in your throat (globus sensation) is fairly common and can be due to a number of things (even something as basic as slight swelling in your throat), so this by itself is not a sign of epiglottis position.
Mike says:
Hello Doctor, just came across this article of yours and have read several others that you’ve written now. As a result of an adverse reaction to a medication, I’ve recently (and suddenly) developed a Central Sleep Apnea as well as some sort of obstructive apnea in the last two months, which I believe is likely a malfunctioning epiglottis. Something in the throat area will “clunk” closed, right as I begin to fall asleep, shutting off the airway and breathing. It has been looked at by a sleep apnea ENT, and he stated the epiglottis itself looked structurally normal, but he admitted it might always be possible for it to do unusual things while sleeping. (He did not suggest a DISE however, and I am unsure if he employs them.)
I’ve just been put on an ASV PAP device for the central sleep apnea, but it is immediately failing as a treatment. As it applies increased positive airway pressure, the blockage in the throat gets *worse* and closes up tighter, and all respiration stops.
I live near you in the SoCal area (Orange County) and am interested in learning how to get better evaluated. (If you think my symptoms sound like possible epiglottis issues.)
Dr. Kezirian says:
Thank you for your comment. I would be happy to see you as a patient. Please contact me via e-mail or contact our office to schedule an appointment. I look forward to speaking with you.
Eric
SAJID KHAN says:
My ENT told me he saw severe Epiglottis prolapse with moderate concentric collapse of my velum. He recommended a combination of UP3 and Hyoid suspension surgery to treat my sleep apnea. I’m not comfortable with traditional UP3 surgery but okay with Hyoid suspension. Am I on the right path?
Dr. Kezirian says:
Thank you for contacting me directly to ask this medical question that is specific to your care. I cannot answer questions like this on the blog.
barry says:
Hi Doctor,
Thank you for this blog. I’ve had sleeping problems for some time and had a DISE
The ENT suggested Epiglottis could be a problem for me and a jaw thrust seemed to keep it out of the way – therefore a MAD should help.
What are you thoughts? Is there anything that look obvious enough to be causing me problems?
Thanks.
Barry.
Dr. Kezirian says:
I removed the Youtube link, as you do not want to share your health information here. An oral appliance could help, but if you really want a telehealth discussion to evaluate your case specifically, you should contact me directly over e-mail (address is on my website).
Zach says:
Hello,
I had a sleep study that came back as 100% central sleep apnea. I saw a cardiologist who said there seemed to be no heart problems, and so then I saw a neurologist. The MRI scan of my brain showed very minor scarring that the neurologist thought wouldn’t be the cause of central sleep apnea, but he noticed that my epiglottis was almost all the way closed as I laid on my back for the scan, and so he suspected that that might actually be the cause of my apnea. My question is this (along with the doctors who are treating me): would it be possible for epiglottal apneas to show up as central apneas on the sleep study if the epiglottis becomes totally closed and the brain simply stops exerting effort? Thanks!
Zach
Dr. Kezirian says:
No. This would not show up as central sleep apnea.
Abigail says:
Hi doctor,
My doctor just found out that my epiglottis is blocking the airway so it’s hard for me to breath at nught. He advised that I do a epiglottis surgery, to remove part of it, around 1/2-2/3. I am worried that I can’t swallow nicely due to the surgery. Should I do the surgery? Is there a long term effect? Or should I just cope with my problem?
Dr. Kezirian says:
These are specific medical questions that should be addressed to your surgeon. Let me know if you would like a formal evaluation from me. For this kind of question, it would ideally include at least a video from your awake flexible endoscopy, if not a drug-induced sleep endoscopy.
Joy says:
If I have surgery on my epiglottis and base of the tongue, could I later have Inspie implant surgery if it didn’t work?
Dr. Kezirian says:
Yes.
Joy says:
Does Inspire have a pending approval with the fda for a model that would accommodate MRI of the torso?
Dr. Kezirian says:
I am not sure if they have something in development, but I have not heard anything from the team at Inspire. You can contact them directly to ask.
Ravi Puralena says:
I did a visit with Dr. K, which was excellent and hugely informative. He was able to refer me to someone in my local area who did a partial epliglotectomy, which was fantastic in giving me my life back. But, what, in my case, was almost as helpful as the surgery was just discovering how to get into the top-secret clinician-only part of my cpap machine (just search on youtube) and disabling the EPR setting on it. Before that my CPAP did nothing and I could feel my epiglottis hitting my throat towards the end of my exhale. After disabling it, I got consistent support from my machine throughout the night.
Lorcan says:
Hello,
I have been suffering with poor sleep for nearly 8 years due to a blockage from epiglotitis. I have visited multiple ENTs, none of which would entertain the idea of performing a partial epliglotectomy which I feel would change my life. They say since I can still breathe
adam's apple feels swollen says:
Thank you so much for this! I believe that this is my sign to visit an ENT.
Clayton says:
Most of this thread regards raising the epiglottis, but I notice as I’m drifting off to sleep that lowering my adams apple (e.g. hum without sound) clears what would otherwise be a blocked exhale. For me, I’m curious if something related to this would explain why CPAP only helps, but does not fix, my ongoing daytime tiredness.
Dr. Kezirian says:
Any activation of muscles around your throat could improve a blocked exhale, although I do think that a blocked exhale may be related more to the soft palate than your epiglottis. When you are asleep, you would not expect the same muscle activation. As for CPAP, there are some patients in whom CPAP appears to push the epiglottis backwards, causing brief but potentially-complete obstruction in your throat. Because it can leave you with airway blockage, in essence your symptoms (daytime tiredness) would continue.