I often hear people refer to someone they know—or themselves—as having “the surgery for sleep apnea”, following it up with the assessment about whether “it worked” or not. Whenever this occurs, I take a deep breath before starting in on the explanation below.
My website hopefully makes it clear that there are many procedures available to treat snoring and obstructive sleep apnea. In spite of the multiple available options, one of my recent studies has shown that over 75% of sleep apnea surgery in the United States is limited to the soft palate alone, shown in blue on the pie chart below (read full article for free here). This study was surprising to many in our field, but the study relied on databases specifically designed to answer these questions and was the most detailed analysis of its kind. The predominance of soft palate surgery is not unique to the United States. Based on my experiences giving lectures in many countries across the world, other countries seem to have an even higher proportion of sleep apnea surgery focused on the soft palate alone.
This study confirmed my suspicion that people pointing to “the surgery for sleep apnea” were likely referring to soft palate surgery, most likely just the surgery first described in 1982 for obstructive sleep apnea: uvulopalatopharyngoplasty (with a name like that, you can see why people just refer to it as “the surgery”). More importantly, this study showed that surgeons also think of this as the only surgical option, and it is no surprise that physicians in other fields have followed suit. These misconceptions are unfortunate, as the field of sleep surgery has come a long way since 1982.
What is the problem with uvulopalatopharyngoplasty for sleep apnea?
Uvulopalatopharyngoplasty, or UPPP, is the most common soft palate procedure. It involves tonsillectomy (if not done previously) and removal of the uvula (tissue hanging down in the back of the throat) and part of the soft palate (the back of the roof of the mouth). This is followed by sewing together the cut tissue edges in the mouth and throat. The good news is that, in high-quality research studies, UPPP has been shown to lower mortality and improve cardiovascular health in patients with severe sleep apnea. Also, most otolaryngologist—head and neck surgeons have been trained to perform it. So UPPP can help patients with obstructive sleep apnea in important ways. This is critical to point out because almost all patients undergoing surgery do not tolerate first-line, non-surgical treatment, so the benefits of surgery must be evaluated against the alternatives, which often means no treatment at all.
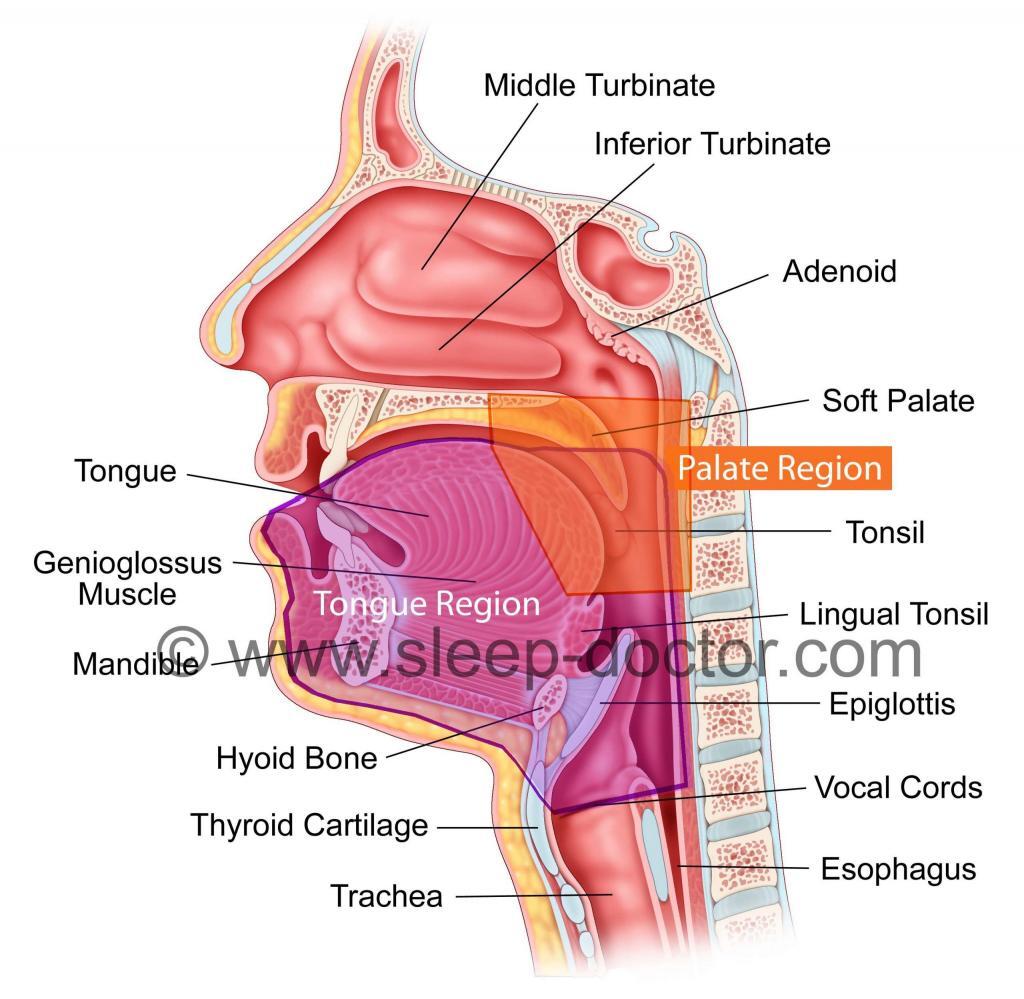
However, we have also learned that UPPP, especially when performed by itself, does not eliminate all sleep apnea in most patients. A major explanation is that the blockage in breathing that occurs in obstructive sleep apnea can occur in the Palate or Tongue Regions (see diagram below). A landmark review of sleep apnea surgery from 1996 (notice the date) showed that patients did much better after UPPP if they seemed to have blockage limited to the Palate Region, without blockage in the Tongue Region. Because blockage in the Tongue Region is common, the past 15-20 years has seen the development of alternative soft palate procedures as well as a number of procedures to treat blockage in the Tongue Region.
Clearly there is room for improvement in the surgical treatment of many patients, but we also have come a long way from 1982 or 1996. I will be speaking at the X World Congress on Sleep Apnea in Rome later this month and then at the American Academy of Otolaryngology—Head and Neck Surgery Annual Meeting in Washington, DC in September specifically on the treatment of blockage in the Tongue Region, evaluation techniques that help in the selection of procedures, and new treatments that are being developed to treat sleep apnea. I look forward to joining my colleagues and sharing our experiences, as we clearly agree on at least one thing:



Milan Kosanovich says:
Dr. Kezirian-
Thank you not only for taking the time to share your specialized knowledge but also for presenting it in such a manner that non-medically trained people can understand & benefit from. I will continue to follow your blog & eagerly await your next entry.
Sleep tight,
Milan Kosanovich
kerry pay says:
I am 61 and completely disabled because no doctor diagnosed my severe osa until I demanded a sleep test. I have severe osa. Two sleep doctors were totally unprofessional regarding Dr. XXXXXXX, who failed to listen to a word I was telling her that her bi-pap diagnosis therapy was not working and another test should be performed as well as a referral to and ENT. She could not even write correctly what I had discussed and she had discussed in my office visits and I left her. I had a second opinion that did another test because my first stated that no pressure prevented my OSA as soon as I entered REM. So he did another titration which confirmed no pressure would prevent my waking up as soon as I entered REM at 60 minutes. My ENT stated after an exam of nose and completely flat palate and nose anatomy problems only thing he would recommend was a tracheostomy. When I returned to him to follow-up he could not remember what he had said in the first consult and now wanted to talk about mouth pieces that he had totally ruled out because of my TMJ and extremely small jaw. When I explained this to my second sleep doctor he even refused to talk to my ENT. I fired both of these doctors and will be referred to you soon because I live in the bay area. I have been complaining of the classic symptoms of OSA since 2001 and no doctor gave me a sleep test or talked about OSA. Thank God for the internet because I have had to be my own doctor because doctors do not listen. They cannot even write correct medical records after I receive a copy the errors are massive;therefore, I send confirm letters as to what has been discussed and treatments. What has happened to the doctors in this country? Thank you so much for putting your info on the internet for college educated patients can investigate medical info so they can hopefully find a doctor who wants the team approach with the patient. All the doctors I have seen become threatened when I try to discuss medical info with them. I do not try to tell them how to be doctors I just want a doctor that “brainstorms” with the patient to reach the best treatment.. Knowledgeable patients should not be considered threats by doctors but should be encourage to learn and help their doctors to reach the best treatment with the patient’s giving the doctor as much detailed symptoms as possible. My doctors that I had before could not even write correctly my symptoms that I was explaining and how it was making me ill.
Thank you and hope to see you at your office soon. My father was a pharmacist, V.P of Sales training at Eli Lilly Headquarters in the 50’s and then had the entire Kaiser account Southern California until he retired in 1975. He taught me to research everything as well as how the medical profession covers up mistakes and patients never find out. All patients just want a caring,compassionate doctor who really thinks thru the symptoms to discover what is going wrong in the body. Sadly the way insurance is allocated now doctors are not given enough time with a patient to listen and take the time to think what the symptoms may cause. A pill is not the answer. My father taught me that anti-biotics are only to be taken if absolutely necessary and most the time they aren’t which is why we now are having resistance because people have been taking too many. Medicine has always fascinated me but I wasn’t good with Latin names. History teacher is my passion but I’m too ill and only sleep 60-120 minutes and am far too tired. Thank you for educating patients because it takes a team!
Ernie Ovies says:
I had my Uvula removed in 1994. My sleep was OK until July of 2011 when I started waking up due to apnea and not being able to fall asleep. The last 18 months has seen a deterioration in my ability to concentrate and I am fatigued all the time. I have contemplated further surgery of the tongue but I am scared of it. I cannot tolerate CPAP and even when I tried it I still wake up after a couple of hours. I tried a mouth device which kept me from snoring for a while but now my wife tells me I am snoring with the mouth device. I cannot beleive something as prevalent as snoring was going to ruin my life
Dr. Kezirian says:
It is definitely reasonable to be scared of surgery, but many patients have told me the recovery was not as bad as they expected (I do make it clear that it will be bad). For tongue surgery, the pain is actually less than after tonsillectomy and/or soft palate surgery. Unfortunately, removal of the uvula alone, while it can help dramatically with snoring, is usually not sufficient for sleep apnea. If you have sleep apnea and cannot tolerate CPAP, you should consider other options. Oral appliances (mouth devices) are potential options, but not all patients are good candidates or able to tolerate them. You should see someone familiar with the range of available sleep apnea procedures. Please contact me at [email protected] if you have additional questions or would like to schedule an appointment.
Vassilka Morrison says:
Thank you for your articles. I am looking for a good doctor to perform surgery since I can’t tolerate CPAP machine. I have TMJ disorder due to removal of too many teeth as a child for braces. I went to a Speech therapist who thinks my tonsils need to come out. She wants me to find a doctor who knows both about surgery and sleep apnea.