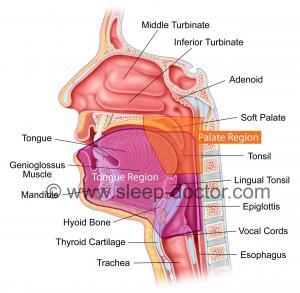
Drug-induced sleep endoscopy (DISE) is an evaluation technique that can be performed for patients with obstructive sleep apnea who are unable to tolerate positive airway pressure therapy (e.g., CPAP or BiPAP). The purpose of DISE is to improve the results of treatment with surgery and/or oral appliances. There are many surgical procedures available to treat the different structures of the nose and throat that can play important roles in causing snoring and obstructive sleep apnea. Successful sleep apnea surgery is based on accurately identifying where the snoring and blockage in breathing is occurring and developing targeted, effective treatment. DISE was developed in Europe over 20 years ago, and it allows surgeons to look inside the throat with a flexible fiberoptic endoscope while a patient is sedated in a way that is similar to natural sleep. Once a patient is sedated but breathing on their own, the surgeon places the endoscope through one of their nostrils and into the throat to examine what are called the Palate and Tongue Regions in the image below. The idea behind DISE is that determining what causes blockage of breathing during sleep will allow surgeons to choose surgical procedures to treat each patient individually rather than just using 1 or 2 procedures for every patient. As one of the world’s leaders in DISE and other evaluation techniques that are essential to selecting surgical procedures, my research has evaluated important characteristics of DISE as a medical test, compared it to other evaluations, showed the importance of experience with DISE, and examined surgical results.
DISE is a somewhat-expensive test in the United States, as it is either performed in the operating room or a procedure suite. In the current era of healthcare reform and the desire to be judicious with spending health care dollars, the questions are whether DISE alters the surgical treatment plan and improves outcomes. A Spanish study published in the August 2014 issue of the medical journal The Laryngoscope addresses the first question. A series of 162 patients underwent a combination of common evaluation techniques performed while patients are awake (basic physical examination, awake endoscopy, and a special X-ray called a lateral cephalogram) and then also DISE. One surgeon developed a surgical treatment plan based on the awake evaluations, and another did so based on the DISE only. The study showed that approximately 40% of patients would have had a different surgical plan based on DISE than they did with the awake evaluations.
The study may overestimate the value of DISE for some patients
When it comes to taking care of patients, this is not exactly what happens. A surgeon will perform awake examinations and then ALSO perform DISE if they feel it is necessary and helpful. It would have been more valuable to have determined the surgical plan before and then after DISE, comparing the two. This is the approach taken by a German group who showed that 78% of patients had a change in treatment recommendation after undergoing DISE. In both studies, many of the changes are related to changes in the open space in the throat after moving the lower jaw forward (Esmarch maneuver), simulating the effect of a mandibular repositioning appliance (also called a mandibular advancement device, one of the types of oral appliances). In the United States, DISE is not a standard evaluation before a patient is treated with an oral appliance. I am not suggesting that they should. Again, DISE is expensive, so a better approach for patients who have a good chance of responding is simply to obtain one, as long as someone believes that they would be able to tolerate it and sleep comfortably while wearing it, every night. There are a number of factors associated with better responses that have been identified in previous studies. (On a side note, a number of dentists are having patients pay to perform all sorts of CT scans or other tests called acoustic pharyngometry based on sound waves before and after advancing their lower jaw. These tests have never, ever been shown to be helpful in predicting whether someone would benefit from a mandibular repositioning appliance and are a waste of time and money–for patients and dentists.)
What do I do when it comes to DISE and sleep apnea surgery?
Although I have performed hundreds of DISE examinations, I am more conservative in its use than my European colleagues who feel the evaluation is a standard part of the workup of every patient with snoring or obstructive sleep apnea. I believe that, by focusing in the surgical treatment of snoring and obstructive sleep apnea, I can make surgical treatment decisions without the need for a separate DISE. I will perform DISE as a stand-alone evaluation (meaning that I do not perform surgery on the same day) in most of my patients, but I will perform DISE at the time of surgery for some patients because it can dictate the type of surgery. For example, I feel that I can decide whether someone will need surgery on their soft palate and tonsils but may use DISE to determine whether I would want to perform the traditional type of palate surgery, expansion sphincter pharyngoplasty, or lateral pharyngoplasty. Similarly, it can dictate how aggressive I need to be when perform lingual tonsillectomy or removing tissue from the back of the tongue.
The Spanish research team indicated that they will continue their work by examining whether DISE improves the results for surgical treatment. There are some well-done studies showing that certain findings during DISE can be associated with better or worse outcomes after certain procedures, but a more-detailed assessment will only help surgeons improve the way they use DISE and work to achieve the best possible results for our patients.




Bob C. says:
First of all, I want to thank you for all the extremely helpful information you provide on your website. It is an amazing resource for people like me trying to find appropriate treatments for obstructive sleep apnea. I have searched through many, many websites regarding OSA and yours, by far, is the most comprehensive and helpful.
I was diagnosed with atrial fibrillation in early 2013 and during a 4-day hospital stay was tested for everything under the sun. There were no clear causes for my afib. (I get to the gym pretty regularly; I’m not obese and have no thyroid issues.) I was referred to a cardiologist and was considering catheter ablation but, thankfully, was told to have a sleep study first. That is how I found out I have OSA. It’s clear to me now that the OSA was the cause of the afib episodes.
With consistent use of CPAP over the course of the past year 15+ months, I recently was able to get off the high risk anti-arrhythmia medication with all its nasty side effects. However, in an attempt to effectively address my OSA for the long term, I have tried all non-surgical treatments and, at this point, I’m at my wits end. I am quite convinced that tongue collapse is my problem. If I sleep on my side, I can get my AHI down to almost zero. (That is, with a contraption on my back — not a long term solution because it is very uncomfortable.) CPAP causes severe bloating/gas but I continue to use it while seeking other remedies. My goal is to resolve my OSA without CPAP.
I met with two ENTs and two oral surgeons and, to my surprise, none of them discussed any type of comprehensive evaluation process/procedure to accurately determine the specific cause of my OSA. Only one of them used a scope to take a peek down my throat. The others simply told me to say “ahhhh” and did a brief visual of my mouth. They all agreed that I have an unusually large tongue base for the size of my jaw; and both ENTs said I was not a good candidate for surgery (< 10% chance of success.) One of the oral surgeons set me up with an oral appliance which did not help me (my tonsils were removed when I was a small child and I have no nasal blockages) the other oral surgeon talked about genioglossus advancement. However, after doing my research, I am apprehensive since there was no thorough evaluation process to substantiate that GGA is the most appropriate procedure for my situation.
After reading your blog post “DISE can change the surgical treatment plan in obstructive sleep apnea” I am only more convinced that I need to find a surgeon that includes an effective physical evaluation before proceeding with OSA related surgeries. Thank you for the post!
Question please… are you familiar with Medtronic’s AIRvance System? (Formerly called Repose.) It is intriguing to me because it involves both genioglossus advancement and hyoid suspension and Medtronic claims it is reversible – furthermore, there is no need to cut a hole through the chin bone for the GGA. I see that you offer both the traditional GGA and separate hyoid suspension but I’m wondering if you can share your thoughts on the AIRvance solution. …Best regards, –Bob C.
Dr. Kezirian says:
Thank you for the e-mail and the kind words. You are correct to seek alternative treatments if CPAP is not working for you. Surgery is not your only option, although it is definitely an option. In focusing in this area, I have developed a thorough evaluation process that can include drug-induced sleep endoscopy. The key to surgery is treating those areas that are most responsible for the blockage of breathing in an individual patient, so that patients are treated as individuals. I am currently at our national academy meeting giving a number of lectures, including one on options to treat blockage of breathing in what I call the Tongue Region on my website. The AIRvance procedure can be helpful for some patients, although I personally do not perform it. The outcomes are roughly similar to what I think of as the less-aggressive options to treat the tongue (tongue radiofrequency, genioglossus advancement), in that it works for patients who are not obese (body mass index below 30). If have a truly large tongue, it may not be the best option for you, as it solely treats patients whose tongue falls backwards without physically reducing tongue size. An evaluation would be required for me to make some of these judgments.
Sandra cox says:
I had not heard of this dise program
Until recently. It sounds like this is exploratory
In terms of my tongue and that based on
Their findings the surgery is recommemded.
How does the surgery work, what other
Options instead of surgery are there. The
Traditional does not work fir me, i cant use
a plate as i have dentures.
Dr. Kezirian says:
We have recently published an international study of drug-induced sleep endoscopy and surgical outcomes. I would suggest that it is not really experimental, although I do not think that every patient considering sleep surgery needs it done. I wrote about this study on my blog at: https://sleep-doctor.com/blog/drug-induced-sleep-endoscopy-findings-are-associated-with-results-of-sleep-apnea-surgery/.
Scott Craig says:
I was reading through your site and noticed this “On a side note, a number of dentists are having patients pay to perform all sorts of CT scans or other tests called acoustic pharyngometry based on sound waves before and after advancing their lower jaw. These tests have never, ever been shown to be helpful in predicting whether someone would benefit from a mandibular repositioning appliance and are a waste of time and money–for patients and dentists.)”. Although I agree with you on the acoustic pharyngometry, there is tremendous value in recommending CBCT not CT to patients considering an oral appliance. I am aware that this procedure is not diagnostic or predictive in nature related to sleep apnea and it’s unfortunate that some organizations teach dentists these types of protocols. However, CBCT’s value in diagnosing craniofacial and other risk-factors associated with sleep apnea and the underline dental health needed to determine candidacy are undisputed in the literature. Further, the data is helpful in identifying comorbid conditions associated with patients suffering from OSA. The information above misleads patients as to the value of a single baseline CBCT and should be updated in my opinion. Additionally, it seems to disparage dentists which is unfortunate as patients need a multidisciplinary team due to the multi-factoral nature of OSA. I hope you reconsider your post and reach out to work alongside you dental colleagues who would greatly benefit in understanding how to identify when to refer to you based on data identified in that baseline CBCT.
Dr. Kezirian says:
Thank you for your comments. First, I would argue that I am most critical of what we do as surgeons, pointing out limitations in the surgical literature because I know it best. I have tremendous respect for many dentists. My grandfather was a dentist, and I have many close dental colleagues who share many of my opinions and concerns. It may be because I practice in a different part of the country, but I am shocked and disheartened by the marketing of largely-untested products or procedures (e.g., AGGA/FAGGA, DNA, ALF) as viable treatments of what is a potentially serious medical disorder. In looking at your website, I see you are not in their camp. You might want to look around at the online marketing claims from your dental colleagues.
Times definitely change, and in the 5 years since I wrote that post, there is some more evidence that measurements obtainable from a CBCT scan may be associated with outcomes of mandibular repositioning appliances. That being said, I am not entirely sure that CBCT scans (occasionally performed as serial scans and not even a single baseline) is required for anyone considering a mandibular repositioning appliance. In my mind, identification of OSA risk factors is not a reason to get a CBCT scan. Like any test, a CBCT scan is useful if it provides information that one cannot easily obtain elsewhere. I believe that experienced, skilled dentists like you can make some of the determinations measured on CBCT scans with physical examination. For example, your examination can likely tell whether a patient has a narrow maxilla without the need for a CBCT scan.
Please feel free to e-mail me directly with any studies that have guided you to perform routine baseline CBCT scans.
John Quidor says:
I was diagnosed with moderate to serve (29 apneas per minute) in July, and tried an oral appliance for more than a month without any good results (I tried it on three different settings, including the tightest). What do you think that means? That the obstruction isn’t in my jaw? Does it makes surgery potentially more or less successful? Thank you.
Dr. Kezirian says:
This just suggests that the oral appliance, at least by itself, is not clearing up your sleep apnea. The fact that you can sleep comfortably wearing your oral appliance is great, as surgery can be performed to add more opening of the space for breathing. I would recommend seeing someone to discuss alternatives or treatments to add to the oral appliance to get the results you need.
kiran says:
My doctor told not to smoke for a week before DISE rest.. is it really require?
Dr. Kezirian says:
I would encourage you to stop smoking entirely. Smoking will interfere with healing from surgery, as it causes swelling that can contribute to sleep apnea.
Hector says:
Do you perform DISE with CPAP? If not, do you know someone that does?
I would like to know if my CPAP failure is being caused by the air pushing my retro-displaced epiglottis down. It seems like the only way to figure this out is with a DISE performed with CPAP.
Dr. Kezirian says:
I do not do this. I have never been convinced it is that helpful. If your CPAP is pushing your epiglottis down, you could have epiglottis surgery, but there are other clues in a complete history and physical examination that would suggest this, starting with a DISE without CPAP.
Ellen Schoffer says:
Thank you for the wonderful information provided. I am struggling with CPAP and was looking into an implant but it is now clear to me that I am not a candidate. As I am from Canada and would have to go to a nearby state, this information saved me a lot of unneccessary costs. Thank you again for a wonderful website.