Drug-induced sleep endoscopy has demonstrated clearly that the epiglottis can play an important role in obstructive sleep apnea in about 5-10% of patients. Surgical treatment approaches suggest that that treatment of the epiglottis specifically can provide substantial improvement in these cases. Multiple procedures have been proposed as options in cases of epiglottis-related obstruction; two of these are hyoid suspension and partial epiglottis resection. In a 2013 post on this blog, I wrote about epiglottis-related obstruction and surgical treatment. In this post, I discuss a new surgical procedure technique called the epiglottis stiffening operation that has some similarities to an approach I have taken for many years.
The epiglottis can cause blockage of the space for breathing during sleep in a few ways. The most common pattern is with the entire epiglottis falling back away from the tongue towards the back of the throat (see below). In many cases, I (and others) have found that patients will often have their epiglottis displaced towards the back of the throat even while awake, making this a clue that the epiglottis may be a major cause of the airway blockage.
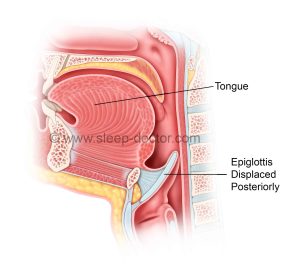
In a 2018 post on this blog, I described our research led by Leslie Irvine, MD showing that the hyoepiglottic ligament may loosen over time, explaining why I see epiglottis-related obstruction more commonly in adults over 60 years of age. The hyoid suspension procedure pulls the epiglottis forward and stabilizes it by holding the hyoid bone forward and relying on a structure called the hyoepiglottic ligament to hold the epiglottis forward too. This procedure can work well, but it requires a neck incision (and therefore a scar) and has some risks, although these are relatively low.
Epiglottis Stiffening Operation: a new technique
In 2019, an Italian group from Humanitas San Pio X in Milan published intriguing results for a new procedure they called the epiglottis stiffening operation in the medical journal ACTA Otorhinolaryngologica Italica. They identified 65 patients with primary epiglottis-related obstruction causing obstructive sleep apnea. Most of them underwent the new procedure with other procedures at the same time, but 14 underwent this new procedure alone. Importantly, they saw no side effects or complications related to the epiglottis stiffening operation across the entire group. Following surgery, they saw clear changes in the position of the epiglottis during office examinations. The epiglottis went from a position towards the back of the throat to one forward closer to the back of the tongue. In addition, there were 5 patients who underwent drug-induced endoscopy after the procedure, and in all cases there was no evidence of epiglottis-related obstruction!
The epiglottis stiffening operation technique involves cauterizing the side of the epiglottis facing the tongue and then allowing the natural healing process to tighten this area and bring the epiglottis forward. In the July 2022 issue of the medical journal The Laryngoscope, they have now published more details about their technique and results in a larger group of patients. They showed specifically where they do and do not treat the epiglottis with cauterization, in addition to numerous other tips and tricks. Among 73 patients with obstructive sleep apnea, the apnea-hypopnea index decreased from 30 to 7 events/hour!
Are the results surprising: yes and no!
The authors point out that they developed this technique based on common knowledge about wound healing, in that a raw area will heal gradually and have tightening, pulling the edges towards the center. By creating this raw area on the one side of the epiglottis, they took advantage of this basic feature of wound healing. Interesting, on my 2013 blog post, a Taiwanese sleep surgeon named Steven Wu, MD, who had spent 6 months as an observer with me, commented about doing something very similar to the epiglottis stiffening operation with a laser. I was unsure how well this would work because there are substantial forces placed on the epiglottis during breathing (awake and asleep) that I thought might limit how much an approach like this would work on its own.
At the same time, for the past 10-15 years I have tried to take advantage of this aspect of wound healing during a procedure called lingual tonsillectomy. This procedure involves removing the tonsil on the back of the tongue (the lingual tonsil) with a controlled cauterization. The area is right next to the epiglottis, and in fact I would extend the dissection onto the epiglottis, effectively doing very similar to the epiglottis stiffening operation in combination with the lingual tonsillectomy. I will admit, however, that I never thought this would work so well for obstructive sleep apnea. I have performed the epiglottis stiffening procedure in a few patients and am happy with it. The recovery is fairly easy for patients, with no major trouble swallowing and relatively little pain, and the results are good. As always, the key is using this procedure only in patients who will have the best chance of success, but that is the art of sleep surgery.
I have added this procedure to my website page on Epiglottis Surgery and will keep you posted on my results.




lawrence nash says:
HI. Do you use this procedure for a floppy epiglottis where an individual is aspirating fluids?
Dr. Kezirian says:
This would not be the right type of surgery for that problem.