This month’s issue of the medical journal Otolaryngology–Head and Neck Surgery included an article written by Emmanuel Jauregui, one of our medical students at the University of California, San Francisco, that reported a case I treated with an unusual complication of hyoid suspension (sometimes called hyoid myotomy and suspension).
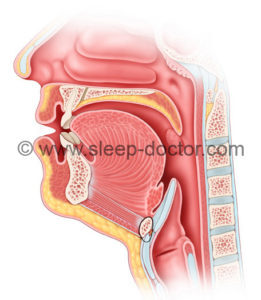
Hyoid suspension is a procedure that can be used to treat obstructive sleep apnea. The hyoid bone is a relatively thin, horseshoe-shaped bone in the neck. The hyoid bone in humans is unique in that it can move. A mobile hyoid bone appears to have been one of the evolutionary changes important in the development of speech, but it likely also contributes to our risks for developing sleep apnea (which is not seen in most animals, except for some dogs). The hyoid bone is important in sleep apnea because it has attachments to a number of other structures, including the epiglottis (through the hyoepiglottic ligament) and muscles that are next to or surround the throat (including the middle pharyngeal constrictor). During sleep, muscles relax, and the hyoid bone is free to move towards the back of the throat, allowing the structures attached to it to fall into the throat and block breathing. The hyoid suspension procedure involves pulling the hyoid bone forward and using stitches wrapped around the hyoid bone to secure it either in a slightly-downward direction to the top part of the Adam’s apple (thyroid cartilage) or upwards to the lower part of the lower jaw (mandible). The image below has the technique I use, to the Adam’s apple.
The unusual complication: new bone formation
The case report discussed a woman who was referred to see me after undergoing the hyoid suspension using the technique with suspension upwards to the lower jaw. She had done well after surgery, but 2 1/2 years later she developed pain, swelling, and drainage from the incision on her neck used for the procedure. After not responding to multiple courses of oral and intravenous antibiotics, she had a CT scan that showed formation of new bone coming from her hyoid bone (the CT scan picture is Figure 1 of the article). We went to the operating room, where we saw that this bone formation had occurred to encase the stitch that was wrapped around her hyoid bone. She recovered uneventfully, and her symptoms also cleared up completely. Emmanuel wrote up the case because this type of new bone formation (called heterotopic ossification) is rare in the head and neck and had never been reported after hyoid suspension. The bone likely formed due to a combination of some trauma to the hyoid bone and chronic infection of the stitch material that did not clear up with antibiotics. During hyoid suspension, stitches are passed around the hyoid bone. Because the hyoid bone is next to the throat (see the figure above), the needle and stitch can pass into the throat, leaving a short length of the stitch sitting in the throat where it is exposed to the normal bacteria we all have there. Because antibiotics are typically used for a few days after hyoid suspension, infection is rare because the lining of the throat will typically heal to cover any exposed stitch material.
The bottom line: do not ignore complications from any procedure
I have written a number of articles and book chapters about complications of sleep apnea surgery, and I have also served as a medical legal expert. I joke that if you are an expert in surgical complications, hopefully you do not have too much experience from complications in your own patients. The truth is that my understanding of complications comes from my own patients and those referred to see me, in addition to the research I have done in the area. My sleep-doctor.com main site includes discussion of procedures and the long list of potential complications for a couple of reasons, including the need for patients to understand these complications but also to let patients know that I am aware of them and take steps to minimize the chance that they occur.
This case above (like another rare case that we published a couple of years ago) highlights the most important thing I stress to patients and surgeons: recognizing complications, discussing them with colleagues if necessary, and determining whether treatment is possible. This patient’s surgeon, instead of ignoring her, had her undergo further evaluation and then sent her for additional treatment. It turns out that one of my own patients had a similar infection (without the bone formation) after hyoid suspension. He also did not respond completely to antibiotics, and I was not sure if removing the stitch would solve the problem. I asked a number of colleagues about this, to no avail, but serendipitously I went to an International Surgical Sleep Society meeting and heard a lecture about hyoid suspension and potential complications from Nico de Vries, a Dutch expert in sleep surgery who is also a good friend. I came home and scheduled the patient for removal of the one stitch (with the technique I use, there are four sutures, so it did not reverse the results), and the infection and drainage cleared up immediately.




Terry says:
Hello, I love the information on your website and I have a few questions. I had a hyoid bone suspension procedure over five years ago, and have been waking up choking and gasping for air off and on in my sleep for over a year. I’ve also been waking up with a fowl taste in my mouth and a nasty coating on my tongue. The following was noted on a recent neck CT scan: “note made of right paramedium 11 mm bony exostosis extending from the ventral aspect of the hyoid bone along the dorsal aspect of the geniohyoid muscle.” Is this something i need to worry about, and could it be causing my choking episodes? Also, if I do need help with this-do you take new patients? Thank you
Dr. Kezirian says:
Thank you for the e-mail. I cannot answer medical questions online to those who are not my patients. You have sent me a direct e-mail, and I look forward to discussing it with you in the office after a formal evaluation.
Craig Huhn says:
I had this surgery a month ago, and recently while yawning felt a hard rip/tear under my chin, which was painful and since then its as though i never had the surgery as my tongue is now fully mobile as it was b4 the surgery. Also my sleep is back to heavy snoring, and waking gasping for air. I asked my doctor that did the procedure about this and he said it was normal and we should wait an additional 30 days to see how things are. My fearvis something is wrong cause since this incident when i turn my head to right and swallow i have a painful bone one bone feeling with in my neck/throat. Are these issues normal, should i be concerned? Thanks Craig
Dr. Kezirian says:
It is not really possible for me to make medical assessments here. It is good that you have spoken with your surgeon. Waiting so early after a procedure is a good idea, although it may be very difficult with the pain you are experiencing.
glen hartsock says:
Hello :
I’m having the ” Hyoid Suspension Procedure “. Could this procedure affect my speech. Pronouncing words?
Dr. Kezirian says:
Any procedure in the nose or throat could theoretically affect your speech, although the risk is pretty low for most procedures. The risk of speech changes after hyoid suspension has not been studied, to my knowledge, but I would expect it to be very low.
D Zamaria says:
I am to have hyoid-suspension possibility with palate surgery in Nov.2018. I was wanting to see if anyone has had this done and or what the outcome was at the time. I have sleep apnea and very tired during the day. I was hoping the above surgery would help with these issues. Any help would be great.
Thank you,
D
Dr. Kezirian says:
Patients are very different, so one person’s experience with a certain surgery or combination of procedures may not be the same as yours. There are places where patients may go more often, such as Reddit, and you may find more answers to this kind of question there.
Christine says:
My son recently had a Sistrunk procedure for a thyroglossal cyst. Since then he snores so loud. What are the options here? I don’t want them to open up his neck again as it’s been operated on twice and the scar is the entire length of the front of his neck. He is 6. The procedure was 3 months ago.
Dr. Kezirian says:
I do not treat children myself, but you should speak with an experienced pediatric otolaryngologist.
Monique says:
I had it done years ago and I keep having discomfort and pain under my tongue. My ENT will not reverse the surgery for me, but I will have to find a way to get this reversed.
I would not recommend this to anyone!!
Dr. Kezirian says:
The hyoid suspension procedure can be “reversed” by cutting the sutures. I have done this a few times for patients with persistent pain or trouble swallowing, and in all cases there has at least been substantial improvement, if not full relief. There are no guarantees, but this is definitely an option. The downside is that you would likely lose much of the benefit of that procedure.
Jeannie Babcock says:
My hyiod bone has been dislocated during a cervical disc replacement and a laminectomy. The surgeon said he moved the bone out of the way. He said forget about it and let it heal. He said no one has ever complained to him about the hyiod bone. I can’t ignore it. I can’t tolerate it much longer. Would I be a candidate for hyiod suspension surgery?
Dr. Kezirian says:
I am not sure what you would mean by a dislocated hyoid bone, as the hyoid bone itself does not have a joint with other bones. Hyoid suspension holds the hyoid in position, but the position is changed. My sense is that the hyoid bone is swollen and painful, but time would probably allow this to settle down. If you have additional questions or specifics, please feel free to e-mail me directly.
Alice Courtney says:
I had an unsuccessful tongue hyiod suspension many years ago (15-20). It didn’t stop my sleep apnea and I developed cellulitis while still in the hospital. That’s just background info. I’m now 72 years old and found out that I have sclerosis sine scleroderma. I noticed today that I have a sore place close to my upper trachea and, upon feeling it, I came to a possible conclusion and would like to pose one question to you: is it possible that something has gone wrong with the apparatus, or that it is being affected by the sclerosis sine scleroderma? I live in Texas, so, coming to see you is out of the question and I no longer see the doctor who performed the surgery..
Dr. Kezirian says:
Anything is possible, but this would not be my first guess about what is going on. I actually do not use the device mentioned in the post myself, but there are surgeons in Texas who do and could therefore comment on this in more detail.
Kevin Green says:
I’m scheduled to have this surgery soon and I am curious about the durability/danger of the stitches. If I were to be struck under the chin is it possible that my hyoid could be damaged or pulled out of place?
Dr. Kezirian says:
I would not think that would be a likely risk.
Morgan Bartley says:
Where to start…..I had this surgery done on March 2nd 2020 and wish I could go back and erase it from being done. For the first week and half it was painful but that was expected. After that mild yawn cause a pop in my jaw that felt like a rubber band snapped in your head. Strangest feeling ever. As COVID-19 lockdown happened to occur during recovery, I have not been able to go back and see my surgeon yet. My side are as follows: difficulty swallowing, can’t look up without keeping my mouth open to do so anymore, acid reflux almost every night, nightly coughing episodes around 2-3 am almost every night, complete loss of feeling from chin down to incision (2 inch by 2 inch patch). It has not been good and my sleep patterns have worsened. Nothing good has come of this so far. Every swallow feels like when you swallow a pill and it gets stuck in your throat except the pill is permanently there. Also from external appearance, I have lost any resemblance of a chin or jaw line. The tension on the line has protruded my neck to the point where i turkey neck and almost no chin definition anymore.
Christian D. says:
I had the hyoid suspension lift nine days ago and as I was eating tonight and open my mouth, I felt like either my jaw popped or one of the stitches had popped on the left side which it is killing me on my ear and left side of my face now. I’m afraid it was a stitch compared to a pop jawbone but not sure. How do I know what’s up going to my follow up in three days If it was the stitch that popped loose.
Dr. Kezirian says:
It is good that you are following up with your surgeon as soon as possible. It is hard to tell exactly what might be occurring, but you should be evaluated.
VickieB says:
I had a hyoid suspension a week ago via hyoid to mandible method. I look like I have the mumps. No chin or jaw definition. I’m told this is normal and that after 4-6 weeks my jaw/neck area should be back to normal appearance. Do you find this is normal and the initial thickening under the chin/neck area does resolve over time?
Dr. Kezirian says:
I do not use this technique. This is one reason. It should improve, as you have some swelling so soon after surgery. You should speak with your surgeon about this.
Tracy says:
I have recently had the hyoid suspension procedure done on March 30th 2021. My question is, I had been experiencing this hair ball sensation in my throat before my surgery and continue to experience that sensation. When I wake up I am still hacking up chunks of phlegm. I have taken 2 steroid packs and antibiotics since my surgery. Any thoughts on this condition or advice moving forward? Thanks
Dr. Kezirian says:
It is still so early after surgery that I would absolutely expect things to improve. You are right to continue to remain in contact with your surgeon through this.
Jenny Brotherton says:
I had hyoid suspension surgery 9 days ago. My OSA is severe, untreated I have 100+ Episodes per hour. With APAP it varies between 30-55. Doc admits he had to tighten really hard to try to give me some help. He also said he hasn’t had a patient swell or experience as much discomfort as I have. My first question, is it possible he tightened too much, as I constantly feel like someone is pulling way too hard on the reins? (Eating and articulating to speak require conscious effort and are exhausting) I’m concerned because it feels like my jaw and alignment are being wracked and TMJ is being aggravated. And secondly, other than cutting the wires and undoing the whole thing, HOW is it adjustable? I have not seen any improvement in my numbers yet (was over 60 with APAP a couple nights ago.) Thank you, I’m having trouble finding information and all my doc has for me is to wait three months and see how it goes.
Dr. Kezirian says:
These are questions that are specific to your case. I cannot provide any insight without have a chance to examine you properly, review your records, etc. I would be happy to evaluate you in person and offer my assessment. I do also offer video consultations (for patients who cannot travel to see me easily), but your case is probably best evaluated by someone who can see you in person (starting with your surgeon but potentially including someone else as a second opinion).