Continuous positive airway pressure (CPAP) is the first-line treatment for obstructive sleep apnea (OSA) in almost all patients in my practice. There are rare cases where I may order mandibular respositioning devices (aka, oral appliances), but CPAP is the primary option, even in patients who specifically request surgical treatment. CPAP has many advantages over alternatives, including the fact that it has very low risks. The challenge, of course, is that CPAP is not comfortable for many patients, in spite of numerous technological advances over the years.
The standard measure of CPAP adherence is usage of at least 4 hours on at least 70% of all days in a 30-day period. While many patients do not experience benefit at this level of usage – and while patients are hopefully sleeping much more than this amount of time – this is an accepted definition of acceptable adherence because studies show that many patients start benefiting with at least this level of CPAP usage.
Most evidence is limited to short-term CPAP adherence
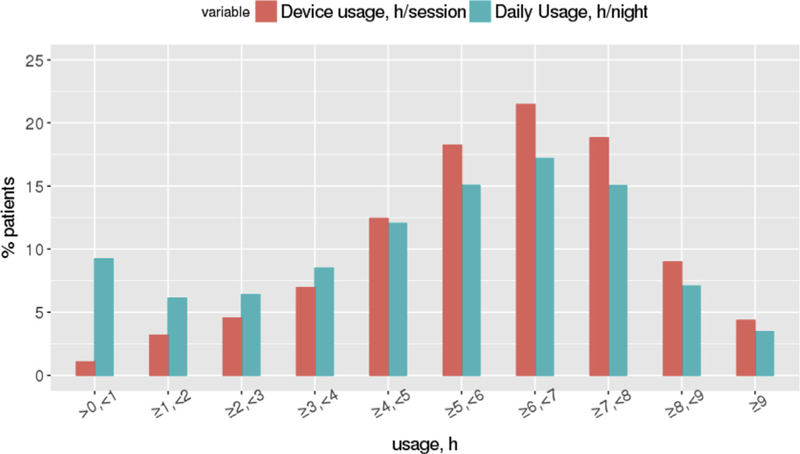
For many years, estimates of CPAP adherence came from self-reports, but these turned out to be inaccurate. Fortunately, the advances in CPAP technology have enabled objective CPAP monitoring, including usage patterns. This allows practitioners to understand adherence in their patients. It has also allowed researchers to evaluate CPAP adherence in large groups of patients and undertake strategies to improve it. Large studies have examined CPAP adherence within the first 90 days of therapy, with a study of almost 2 million patients from the ResMed cloud platform suggesting that 75% of patients were adherent. The overall distribution of CPAP adherence is presented below:
Additional research with ResMed data suggested that patient engagement strategies can improve short-term adherence to 87%, although this excluded many patients who stopped using CPAP within the first week of use.
What about longer-term CPAP adherence?
This looks encouraging, and this figure is the number we often quote to patients. However, what we really care about is how well our patients do over many years, not just the first 90 days. There are some studies using self-reported data, suggesting that adherence declines over time. However, we now can use objective data that are available to understand usage patterns over time. In this month’s Journal of Clinical Sleep Medicine, a Korean research group examined CPAP adherence in 187 study participants who started on CPAP from 2018-20. They showed that adherence rates at 3 months and 12 months after CPAP initiation were 79% and 51%! Adherence at 3 months was associated with greater age and OSA severity (apnea-hypopnea index), but adherence at 12 months was associated with the degree of oxygen desaturation and symptoms such as nasal obstruction and awakening from sleep.
What does this mean?
This study is important, for many reasons. First, it uses objective measurement of longer-term CPAP adherence, as opposed to self-reported usage that is found in other studies. It is therefore unique. Second, it suggests that 12 month adherence rates may be substantially (!) lower than at 3 months, with enormous implications for OSA management on a population basis. Third, factors associated with longer-term adherence may be very different than those associated with short-term adherence. Finally, it points to the need for additional research to characterize longer-term CPAP adherence (ideally much longer than 12 months after the start of treatment) and the factors associated with adherence. This will, in turn, pave the way for research on interventions that can improve CPAP adherence.
I am a sleep surgeon who is committed to treating patients who cannot tolerate CPAP in spite of our best efforts. Part of this is making sure we are putting forth our best efforts to improve CPAP adherence, and this all starts with learning as much as we can about how to do so. I hope the sleep medicine field greets this recent study with enthusiasm and embraces the challenge to do our best. I look forward to learning more from my colleagues.




+ 9 = 11