Surgical treatment of obstructive sleep apnea depends on determining where blockage of breathing is occurring during sleep, whether in the Nasal, Palate, or Tongue Regions that I outline on my main website: sleep-doctor.com. Often an individual will have more than one of these Regions involved, leading to my recommendation of a combination of surgical procedures. One of the most common questions I receive is whether a more-limited approach would be successful in treating sleep apnea, particularly surgery focused only on the nose.
Why should someone with sleep apnea consider nasal surgery?
There are 3 reasons to undergo nasal surgery (after an unsuccessful trial of medications) if someone has obstructive sleep apnea:
- Improving nasal obstruction broadly
- Improving nasal obstruction during the night so that other treatments such as positive airway pressure therapy (for example, CPAP) and oral appliances will work better
- To improve sleep apnea with surgery as a primary treatment
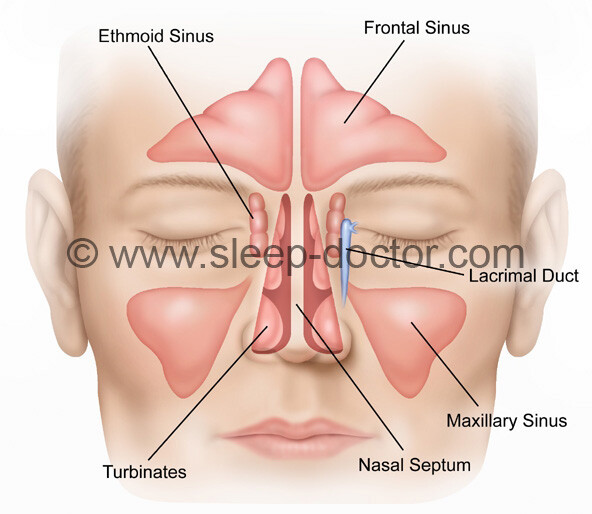
There are many studies showing that nasal surgery–whether of the nasal septum, turbinates, sinuses, or the outside of the nose–can improve nasal obstruction and other related problems. In addition, improving nasal obstruction is one of the few things that has been shown to improve results of treatment with positive airway pressure therapy, and my experience is that it can do the same for oral appliances.
So what about nasal surgery as treatment of sleep apnea by itself?
Likewise, there are many studies evaluating the impact of nasal surgery by itself in the treatment of sleep apnea. However, many of the studies are fairly small, leading to challenges in drawing clear conclusions. This type of research evidence lends itself well to the technique of meta-analysis, the scientific combination of results of many studies into one larger study. The September 2015 issue of Otolaryngology–Head and Neck Surgery includes a published meta-analysis on this topic. In short, the study showed that nasal surgery can improve important symptoms such as sleepiness and a measure of sleep apnea called the respiratory disturbance index (capturing incomplete blockage of breathing that is enough to wake up someone from sleep) but does not generally achieve a significant improvement in the apnea-hypopnea index that measures more-substantial blockage of breathing. For anyone interested in hearing more, the journal has posted a podcast concerning the meta-analysis and the perspectives from Dr. Lisa Ishii (lead author) and me.
What do I tell my patients?
When it comes to nasal surgery alone for sleep apnea, the impact likely depends on a number of factors:
- severity of nasal obstruction and the improvement that occurs after treatment (bigger improvements make a bigger difference)
- the degree of sleep apnea (mild obstructive sleep apnea has a better chance of clearing up than does moderate to severe sleep apnea)
- unhelpful changes in breathing patterns caused by nasal obstruction, such as mouth breathing
- any other obvious sources of blockage of breathing that are not treated with nasal surgery
However, I have no crystal ball. Based on a personalized approach to shared decisionmaking with patients, even when the chances of clearing up sleep apnea are low, sometimes I will treat nasal breathing as a first step and reevaluate before proceeding with additional procedures. Sometimes we are all surprised by how much benefit we see after nasal surgery.




Matthew J Wright says:
Hi Sir
I’m Matthew Wright. Just a concern veteran enquiring about ways to decrease the level of my obstructive sleep apnea. According to what Im reading the nasal surgery can reduce the level to help you breath better or your treatment work better. As a result, it reduces it from obstructive Level to mid or mile.
Dr. Kezirian says:
Nasal breathing alone is usually not the main cause of obstructive sleep apnea, but it can be if the nasal blockage is really bad and if the obstructive sleep apnea is mild. If you have moderate to severe obstructive sleep apnea, treating your nose may or may not improve the sleep apnea on its own, so I would not say that it would clearly make your sleep apnea mild. However, there are many potential benefits of treating the nose, including making it easier for you to tolerate other treatments (as you correctly point out).